Surgical Intervention
Arterial Events
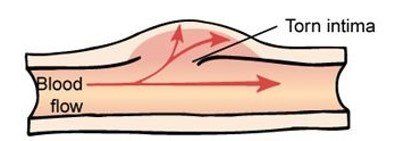
Many symptomatic arterial events are dissections that are self-limiting and may not require radiologic intervention or surgery. In the case of arterial rupture, urgent repair by any possible means is required. Not all dissections are symptomatic. Indeed, it is not uncommon to discover silent arterial defects during routine arterial monitoring.
Symptoms of arterial dissection may be pain secondary to the tear in the arterial wall, to capsular stretch, or related to ischemia in organs or limbs located distal to the dissection. Locations that are commonly symptomatic are iliac and femoral arteries, mesenteric and celiac vessels, renal arteries, aorta (any location), and peripheral arteries of the limbs.
Acute management of symptomatic dissection requires pain control, blood pressure control, and monitoring for signs of deterioration in case of ischemia. Anticoagulant or antiplatelet therapy may be required when there is a high risk of ischemia due to narrowing of the vessel or peripheral embolisation. Given the risk of complication due to these therapies, their use is generally limited to a short period of time. In the event of arterial rupture, interventional therapy may be indicated.
Anatomically contained (partial) ruptures may be treated medically but require close monitoring to detect recurrent bleeding.
Non-contained ruptures or clinically unstable aneurysms (pre-rupture) or false aneurysms most often require intervention. According to the location, interventional radiology or open surgery may be indicated, although invasive procedures may be more likely to provoke further morbidity.
The nature of treatment depends on the location of the arterial rupture. Often occlusion by embolization of the bleeding artery is necessary. The best setting for vascular surgery is the planned repair of aneurysms and dissecting aneurysms, especially those affecting the aorta or iliac vessels. Open intervention however requires specific repair techniques because of the inherent vessel friability and should be avoided as much as possible.
Management of Dissections and Aneurysms in VEDS was presented by Dr. Sherene Shalhub, University of Washington, on December 9, 2019, as part of The Marfan Foundation's Prepare for Victory: Virtual Medical Symposium Series.
Repeated Arterial Events
Patients with symptomatic arterial events may present during the acute phase of their dissection/rupture with repeated arterial accidents in distant arterial territories in the hours/days following the initial event.
The risk of secondary accidents may increase with the severity of the initial event, the length of the hospital stay, the invasive character of treatment, and the extent of fluid overload. No specific causal factors have been formally identified to explain these events.
It is suggested a protocol of “permissive hypotension” in which hypotension is permitted as long as it does not compromise intellectual or other organ function, the avoidance of inotropic agents, and the judicious use of IV fluids to increase pressure.
Additional precautions are required with indwelling catheters because of the risk to the integrity of vascular or organ walls.
James Black, MD, Associate Professor of Surgery & Vascular Surgery and Endovascular Therapy
Aneurysm
The artery dilates to form a swelling with all 3 layers intact. However where the artery wall has ballooned out to form the aneurysm, there is chance that the artery wall may rupture.
Evaluation
Evaluation at the time of emergency referral depends on the signs and symptoms. In general, non-invasive evaluation of the abdomen, chest, and head are preferred using MRI, CT, and venous angiographic approaches to understand blood loss.
Use of arteriography with high pressure injection is generally avoided because of the risk of further vascular injury. Some vascular events can be dealt with effectively with embolization. Although covered stents are being placed in life-threatening situations to forestall active bleeding, it is not known if and how arteries will withstand the pressure of the stents over the long course.
Aneurysmal dilation may occur in some while others may require open surgical intervention. Bowel rupture almost always requires surgical intervention and usually leads to isolation of the distal bowel, removal of the ruptured segment, and creation of a colostomy. Repair of colostomy has become more commonplace and is frequently successful.
Recurrent surgery may be associated with ilio-colic fistula formation and subtotal colectomy may prevent further colonic ruptures. This possibility could be discussed at the time of the first colonic rupture if the diagnosis of vascular Ehlers–Danlos syndrome has been established.
Source: Byers PH, Belmont J, Black J, De Backer J, Frank M, Jeunemaitre X, Johnson D, Pepin M, Robert L, Sanders L, Wheeldon N. 2017. Diagnosis, natural history, and management in vascular Ehlers–Danlos syndrome. Am J Med Genet Part C Semin Med Genet 175C:40–47. Images are generic.
Treatment
Treatment is first given is to control your blood pressure and heart rate, usually in the emergency room.A CT angiogram is used to determine the location and extent of the dissection, and to evaluate what part of the aorta and which aortic branches may be involved.
If endovascular treatment is appropriate, one of the two procedures below will likely be recommended.
TEVAR or stent grafting is a minimally invasive treatment for an aortic dissection or aneurysm. In the case of a dissection, a cloth-covered stent graft is used to seal the tear in the aorta. One or more uncovered stents may be added to support and expand the true lumen in order to improve blood flow to your abdominal organs, pelvis and legs.
- You will be sedated or be given general anesthesia.
- Once you are comfortable, a puncture will be made in a femoral artery. With the help of X-ray images, guide wires and a thin tube (catheter) are advanced through the artery to the dissection.
- Angiogram images of the aorta are taken to decide where the covered stent should be placed. The stent graft is then advanced into position.
- Confirming X-rays are taken. If needed, the covered stent is adjusted to form a seal. Additional angiogram images are taken to confirm whether the position and length of the covered stent is adequate or additional uncovered stents are needed. Intravascular ultrasound may also be used to assess progress.
- After all needed stents are in place, any wires or catheters are removed and access punctures or wounds are closed.
ENDOVASCULAR FENESTRATION is done to improve blood flow to a specific branch artery or to help equalise pressure between the true and false lumens.
- You will be sedated or be given general anesthesia.
- Once you are comfortable, a puncture will be made in a femoral artery. Through the puncture, the vascular surgeon inserts a thin tube (catheter) and administers blood thinners. Assisted by X-ray images, a wire and angled catheter are advanced to the affected area.
- Angiogram images are taken to find any natural holes (fenestrations) in the dissection flap. If no holes are found, the vascular surgeon will create one.
- Under X-ray guidance, a wire is sent through the true lumen, across the dissection flap to the false lumen. Another angiogram or intravascular ultrasound is taken to confirm progress.
- A balloon angioplasty is performed to enlarge the hole/s. A support stent may be placed (stented fenestration) to assist blood flow through the enlarged hole. This may help normalise pressure across both sides, and improve blood flow to organs and legs.
- After all needed fenestrations have been created, wires and catheters are removed and access punctures or wounds closed.
Source: Dr. Virendra I. Patel, Society for vascular surgery.